Understanding e-sigara: a practical look at the effects of vaping
This comprehensive guide explores e-sigara usage and clarifies what e cigarettes do to your lungs, focusing on both short-term reactions and long-term risks. The goal is to give readers reliable, actionable information so they can recognize warning signs early and make informed decisions about inhaled nicotine and aerosolized additives. The content below is structured for clarity: we begin with a plain-language overview, then dive into the science of inhaled aerosol, list clinical signs and symptoms to watch for, describe common diagnoses linked to vaping exposures, review diagnostic tools and tests clinicians use, and close with prevention, cessation tips, and policy considerations.
Quick overview: how vaping differs from smoking
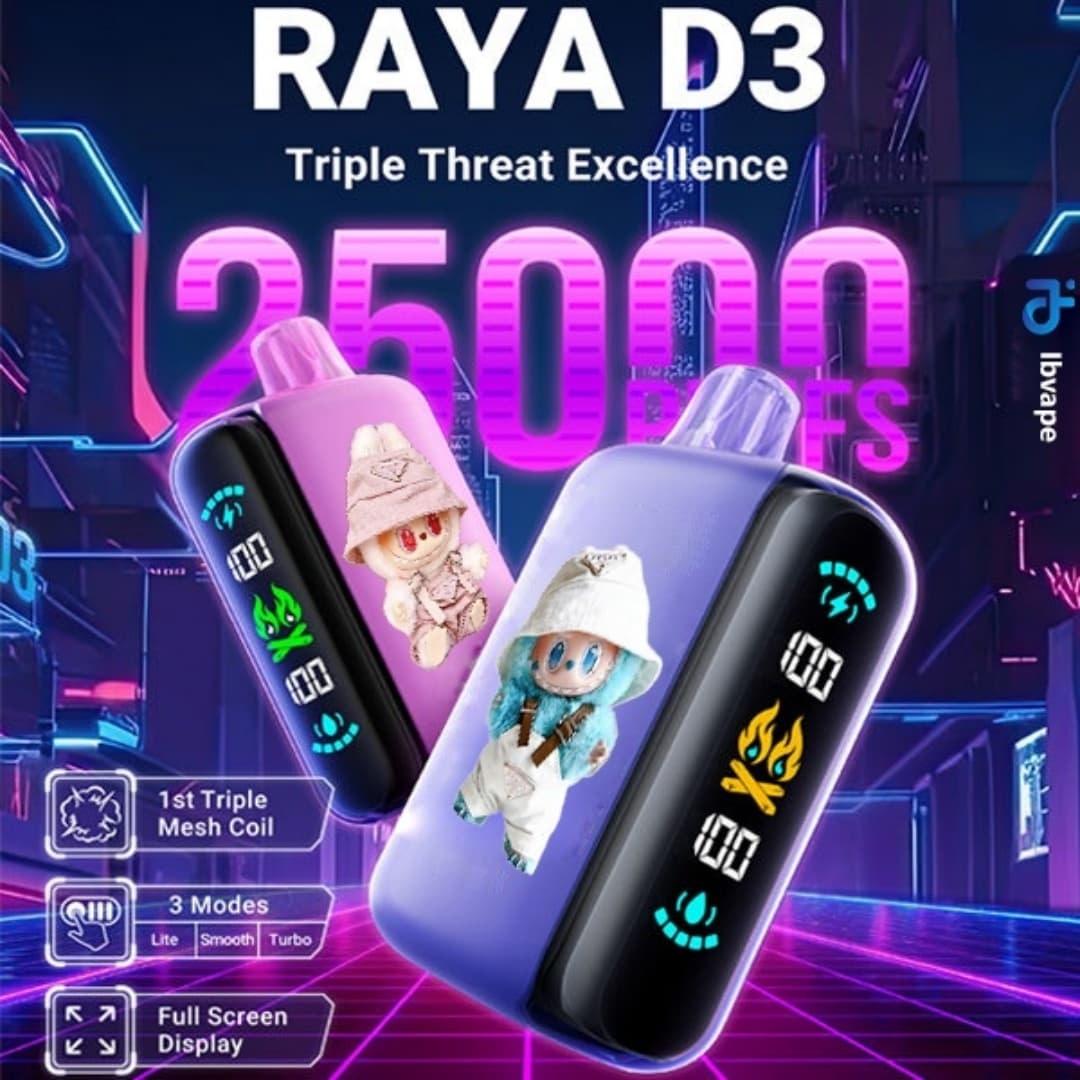
Vaping devices, marketed under many brand names including e-sigara, heat a liquid (commonly called e-liquid or vape juice) into an aerosol that users inhale. The what e cigarettes do to your lungs question centers on what that aerosol deposits in delicate respiratory tissue. Unlike cigarette smoke, which comes from combustion and contains tar and thousands of combustion byproducts, vaporized e-liquids create ultrafine droplets carrying nicotine, solvents such as propylene glycol (PG) and vegetable glycerin (VG), flavoring chemicals, and sometimes heavy metals released from device components. These constituents interact with the airway lining, triggering inflammation, altered immune responses, and in some cases, direct chemical injury.
Key components of e-liquid and why they matter
- Nicotine: A potent stimulant and addictive compound that affects respiratory mucosa and systemic cardiovascular function. Nicotine alters ciliary function and can impair airway clearance.
- Solvents (PG, VG): Generally recognized as safe for ingestion, but inhaled repeatedly they can dehydrate mucous membranes and carry flavoring chemicals deep into the bronchioles.
- Flavoring agents: Thousands of compounds are used to create flavors; some, such as diacetyl and acetyl propionyl, have been associated with bronchiolar scarring in occupational exposures.
- Ultrafine particles & metals: Aerosol particles can reach deep alveoli and deliver metals like nickel, lead, and chromium that can promote oxidative stress.
- Thermal decomposition products: Heating elements can generate formaldehyde, acetaldehyde, acrolein and other volatile organic compounds that are irritant or toxic to lung tissue.
Biological mechanisms: how inhaled vapor affects lung tissue
The respiratory tract is lined by airway epithelium, cilia, mucus, and resident immune cells. Exposure to e-cigarette aerosol can produce:
- Acute epithelial irritation and surfactant disruption, impairing alveolar stability.
- Oxidative stress from reactive oxygen species triggered by chemicals and metals, which can damage DNA and cellular membranes.
- Pro-inflammatory signaling that recruits neutrophils and macrophages, potentially leading to persistent inflammation.
- Altered macrophage function, reducing pathogen clearance and increasing susceptibility to infections.
- Fibrotic processes in susceptible individuals: repeated injury and aberrant repair can lead to scarring and fixed airflow limitation.
Common clinical signs and symptoms to watch for
Individuals who vape may experience a range of respiratory complaints. Some symptoms are acute and reversible after stopping exposure; others may indicate a more serious process requiring medical evaluation. Be alert for:
- Persistent cough lasting more than two weeks or cough that progressively worsens.
- Shortness of breath with exertion or at rest, especially if it represents a change from baseline fitness.
- Chest pain or tightness that is new and reproducible with breathing.
- Wheezing or high-pitched noises during breathing.
- Recurrent respiratory infections or slow recovery from bronchitis-like illnesses.
- Unexplained fatigue, weight loss, or fever accompanying respiratory symptoms, which may indicate inflammation or infection.
When symptoms are urgent
Seek immediate medical care if there is severe shortness of breath, bluish lips or face, fainting, or rapidly worsening chest pain. In the context of heavy or recent vaping, clinicians will consider emergent causes such as acute chemical pneumonitis, severe asthma exacerbation, or EVALI (e-cigarette or vaping-associated lung injury).
Recognized diagnoses related to vaping and inhalation injuries
Clinicians and researchers have documented several patterns of lung injury linked to inhaled aerosols, including those from devices marketed as e-sigara. These include:
- Acute lipoid pneumonia: Sometimes associated with inhalation of oily substances or lipid-containing aerosols; presents with cough, fever, and infiltrates on imaging.
- Bronchiolitis obliterans (obliterative bronchiolitis, “popcorn lung”): Peripheral small-airway fibrosis historically linked to diacetyl exposure; causes progressive dyspnea and fixed airflow obstruction.
- Acute eosinophilic pneumonia: Rapid-onset respiratory failure with eosinophilic infiltration of the lungs, sometimes following a new inhalational exposure.
- Diffuse alveolar damage / ARDS: Severe chemical injury can produce widespread alveolar compromise requiring intensive care.
- EVALI: A syndrome described in recent years characterized by hypoxemia, bilateral infiltrates on chest imaging, and often a history of vaping; vitamin E acetate and other contaminants have been implicated in many cases.
How clinicians evaluate suspected vaping-related lung harm
Evaluation typically includes a focused history (timing, device type, product source, frequency, and concurrent tobacco use), physical exam, and targeted investigations:
- Chest X-ray and chest CT: CT scanning provides detailed views of airway and parenchymal patterns, identifying ground-glass opacities, consolidation, or small-airway changes.
- Pulmonary function tests (PFTs): Spirometry, lung volumes, and diffusion capacity (DLCO) assess airflow limitation and gas exchange, helping distinguish obstructive from restrictive patterns.
- Blood tests
 : Inflammatory markers, complete blood count with differential (to detect eosinophilia), and infection screening.
: Inflammatory markers, complete blood count with differential (to detect eosinophilia), and infection screening. - Bronchoscopy with bronchoalveolar lavage (BAL): Allows sampling of alveolar cells and testing for lipid-laden macrophages, infectious organisms, and chemical exposure markers.
- Specialized toxicology: When available, testing for components such as vitamin E acetate, specific flavoring agents, or metals in BAL fluid or vapor condensate can clarify causation.
What the research says about long-term risk
Longitudinal data are still emerging because modern vaping products have only been widespread for a decade. However, animal studies, cellular experiments, and observational human data suggest plausible long-term harms: increased risk of chronic bronchitis symptoms, persistent small-airway disease, impaired bronchial clearance, and cardiovascular effects that secondarily influence pulmonary health. Dual use of cigarettes and vaping devices may compound harm. Public health authorities caution that inhaling aerosolized flavor chemicals and additives is not benign, and the safest option for lung health is to avoid inhalation of these products entirely.
Practical steps to protect your lungs
Whether you are a current user of e-sigara or advising someone who vapes, consider these harm-reduction and prevention tips:
- Stop vaping if you develop concerning symptoms. Early removal of exposure often leads to improvement in inflammatory conditions.
- Avoid modifying devices (open systems, adding oils, heating at higher temperatures) because these changes can increase production of toxic compounds.
- Use regulated products only and avoid illicit or black-market cartridges, which have been linked to many severe EVALI cases.
- Seek medical evaluation for persistent cough, breathlessness, or chest pain; describe all inhalational exposures frankly to the clinician.
- Consider nicotine replacement or evidence-based cessation supports if quitting nicotine is the goal—behavioral counseling and pharmacotherapy can increase success rates.
Diagnostic red flags for clinicians
Clinicians should maintain a high index of suspicion when encountering patients who vape and present with hypoxemia, bilateral imaging abnormalities, elevated inflammatory markers, or BAL findings suggestive of chemical injury. Early multidisciplinary management (pulmonology, toxicology, infectious disease) is often warranted for moderate-to-severe presentations.

Special populations: youth, pregnant people, and those with chronic lung disease
Young people who vape risk nicotine dependence during critical brain development windows; their lungs may also sustain damage during growth. Pregnant people who inhale aerosols expose the developing fetus to nicotine and possibly other teratogenic compounds, raising concerns for perinatal outcomes. Individuals with asthma, COPD, or other chronic respiratory conditions can experience exacerbations and should be counseled to avoid vaping entirely.
How to document exposures and communicate risk
Careful documentation helps both clinical care and public health surveillance. When asking about exposures, include:
- Brand or product names (including e-sigara if applicable), device type, and frequency.
- Sources (retail, online, informal dealers) and whether cartridges were altered.
- The presence of oils or additives, especially vitamin E acetate or other lipophilic substances.
Clear counseling should balance empathy for nicotine dependence with candid information on risks and available supports for quitting.
Lifestyle, recovery, and rehabilitation
After an acute injury, many patients benefit from pulmonary rehabilitation, breathing exercises, and strategies to restore fitness. Smoking cessation programs, digital supports, and follow-up PFTs at intervals help monitor recovery. Nutrition, vaccination (influenza, pneumococcal), and avoidance of respiratory irritants support respiratory resilience.
Policy, regulation, and public health context
Regulatory frameworks vary by country, but public health agencies have emphasized restricting youth access, banning certain flavorings, and enforcing product testing. Surveillance systems tracking cases of vaping-related lung injury (including those linked to e-sigara products) remain critical for timely identification of hazardous additives or manufacturing defects.
Practical messaging for families and communities
When discussing vaping risks with family members, emphasize avoidant language (what to avoid), recognize that curiosity and youth-targeted marketing are drivers of uptake, and provide resources for quitting. Schools and community programs can play an active role by combining education with access to cessation help.
How to talk to a healthcare professional about vaping-related symptoms
Be prepared to describe the product (name, frequency, device), the onset and pattern of symptoms, any self-treatment attempted, and other risk factors such as asthma or immunosuppression. If possible, bring the device or packaging to the appointment to assist clinicians in identifying components for testing.
Summary: balanced, evidence-informed approach
In short, detailed answers to what e cigarettes do to your lungs depend on product composition, frequency and pattern of use, device characteristics, and individual susceptibility. The available evidence indicates that inhaling vapor is not harmless: it can provoke airway inflammation, impair defense mechanisms, and in some cases cause acute or chronic lung disease. Minimizing exposure, recognizing the signs listed above, and seeking medical review early are the best strategies to protect respiratory health.
Resources and next steps
For those ready to quit or seeking more information: consult local smoking cessation services, visit national health agency websites for evidence-based guidance, and speak with a primary care clinician or pulmonologist when symptoms are present. If you suspect an acute vaping-related injury, emergency care may be necessary.
FAQ
Q1: Can occasional vaping cause permanent lung damage?
A1: Occasional use is less likely to cause irreversible change than heavy, prolonged exposure, but even infrequent vaping can trigger acute reactions in susceptible individuals and may contribute cumulatively to long-term risk; the absence of immediate symptoms does not guarantee safety.
Q2: How is EVALI different from classical pneumonia?
A2: EVALI often presents with bilateral infiltrates and hypoxemia and may be linked to inhalational toxicants like vitamin E acetate; cultures are usually negative for a single infectious organism, and clinical history of recent vaping helps distinguish it from infectious pneumonia.
Q3: If I stop vaping, will my lungs heal?
A3: Many inflammatory changes improve after stopping exposure, especially early on. Degree of recovery depends on the extent and duration of injury; pulmonary rehabilitation and medical follow-up aid recovery.
Note: This article provides general information and does not replace medical advice. If you are concerned about symptoms or exposures, contact a healthcare professional promptly.